What is research?
Children's cancer research focuses on understanding, improving treatments, and finding cures for cancers that affect children. Some research projects also look to enhance a patient’s quality of life during and after treatment. Research is important because knowledge shapes how we diagnose, treat, and improve the lives of children with cancer.
Translational Research Pipeline
Taking research from ‘Bench to Bedside’ can also be referred to as the Translational Research Pipeline.
This research pipeline is the process of turning ideas from the lab into real treatments for childhood cancer patients. It starts with studying cancer cells to understand how they work and what makes them grow. Researchers then try and find ways to stop or destroy these cancer cells. They also look to see if these treatments are going to be harmful to other non-cancerous cells in the body.
Once a potential treatment approach is identified, it is tested on different models of cancer before it is tested in human to make sure it is safe and effective. Once deemed safe and effective, a treatment requires approval from a number of bodies, including the Human Research Ethics Committee (HREC), the Clinical Trial Notification (CTN) or Clinical Trial Approval (CTA) scheme, and in some cases, the Therapeutic Goods Administration (TGA).
If the treatment approach is demonstrated to be better and/or safer than the existing treatment, it is then utilised as “standard care” in the clinic.
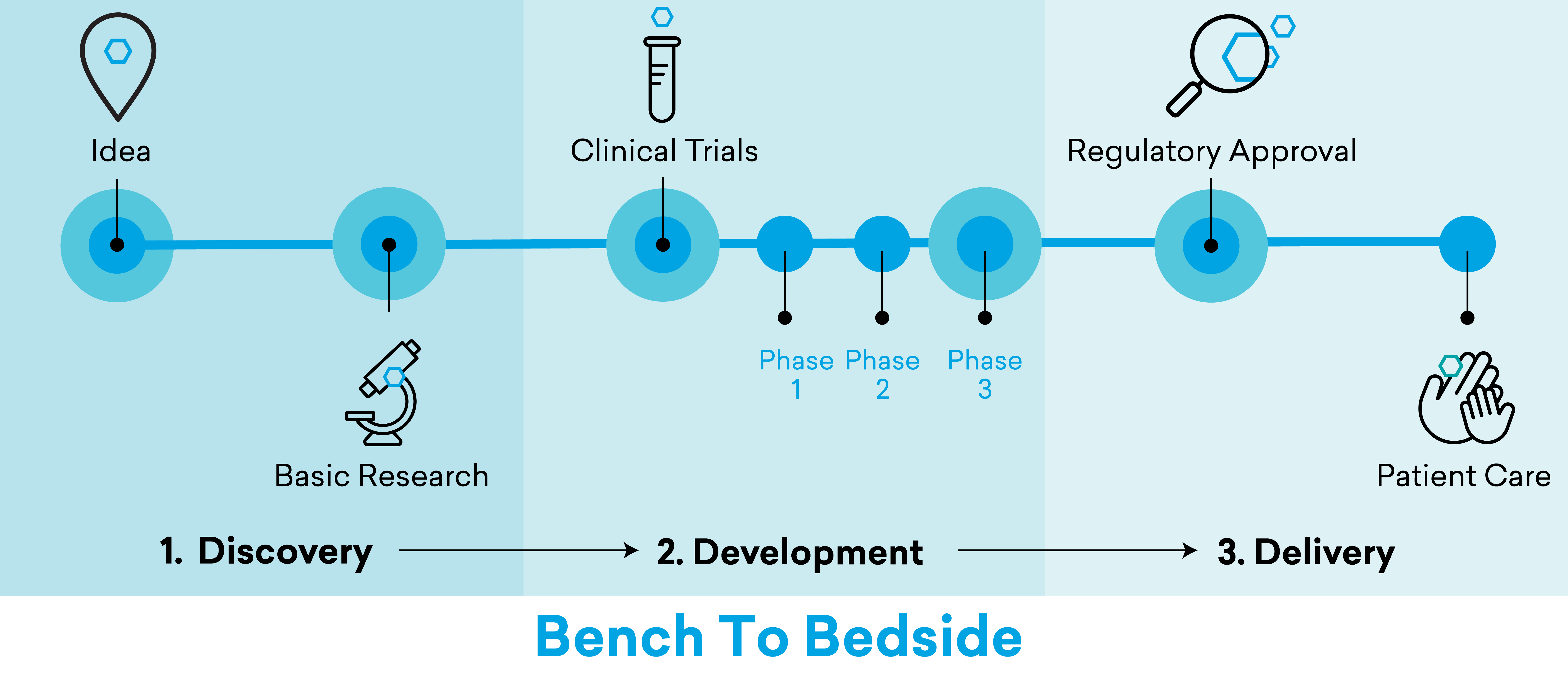
It takes many years for a treatment strategy to pass through the pipeline. It roughly takes three-to-six years to truly understand a how a cancer cell functions and identify new targets and validate that these targets are effective.
It then takes another six-to-seven years to test a hypothesis or treatment on a human being and for it to pass through the various clinical trial phases. Another two-to-five years is required to finally review and approve a treatment for widespread clinical use
While some research projects make it all the way down the pipeline, others do not, because a treatment either is not effective or is not safe for human use because there are too many different reactions or side effects from those who use the treatment.
Researching beyond a disease
Childhood cancer research is shifting to focus on the whole patient, not just the disease. This means addressing long-term side effects, managing symptoms, and helping children reintegrate into society and live healthy, fulfilling lives.
Cancer treatments often cause late effects and long-term health issues that may appear months or years after treatment. These effects can be physical, like problems with growth, fertility, or organ function; psychological, affecting mental health; or immunological, weakening the immune system. While some of these effects can be predicted, others are unexpected. Regular follow-up care and screenings are important, because they help to monitor and manage these issues.
Some research programs aim to reduce these late effects and improve survivors' quality of life. This includes finding ways to predict and minimise side effects, supporting mental health, improving physical fitness, and helping children catch up in school. Supportive care programs are also being built into treatment plans to ease the transition from active treatment to life beyond cancer.
For many children, life after cancer involves adapting to a "new normal," shaped by the long-term impact of treatments and worries about the future. Continued care, including follow-ups and guidance on managing late effects, is critical. Relapse remains a possibility for some children, driven by biological, environmental, or treatment-related factors. Ongoing research explores alternative treatments to improve outcomes for those who don’t respond to current therapies.
The Kids’ Cancer Project has funded numerous programs to help childhood cancer survivors thrive both during and after treatment.
There are many different types of research that focus on different aspects of the cancer journey, because there are so many things that are part of that pipeline
While many researchers are based in the labs trying to understand how cancers form and then trying to kill those cells, others are exercise physiologists and nurses trying to help patients with rehabilitation or symptom management.
The Kids’ Cancer Project supports research into childhood cancer from diagnosis and treatment to survivorship and beyond.
Read more about these projects
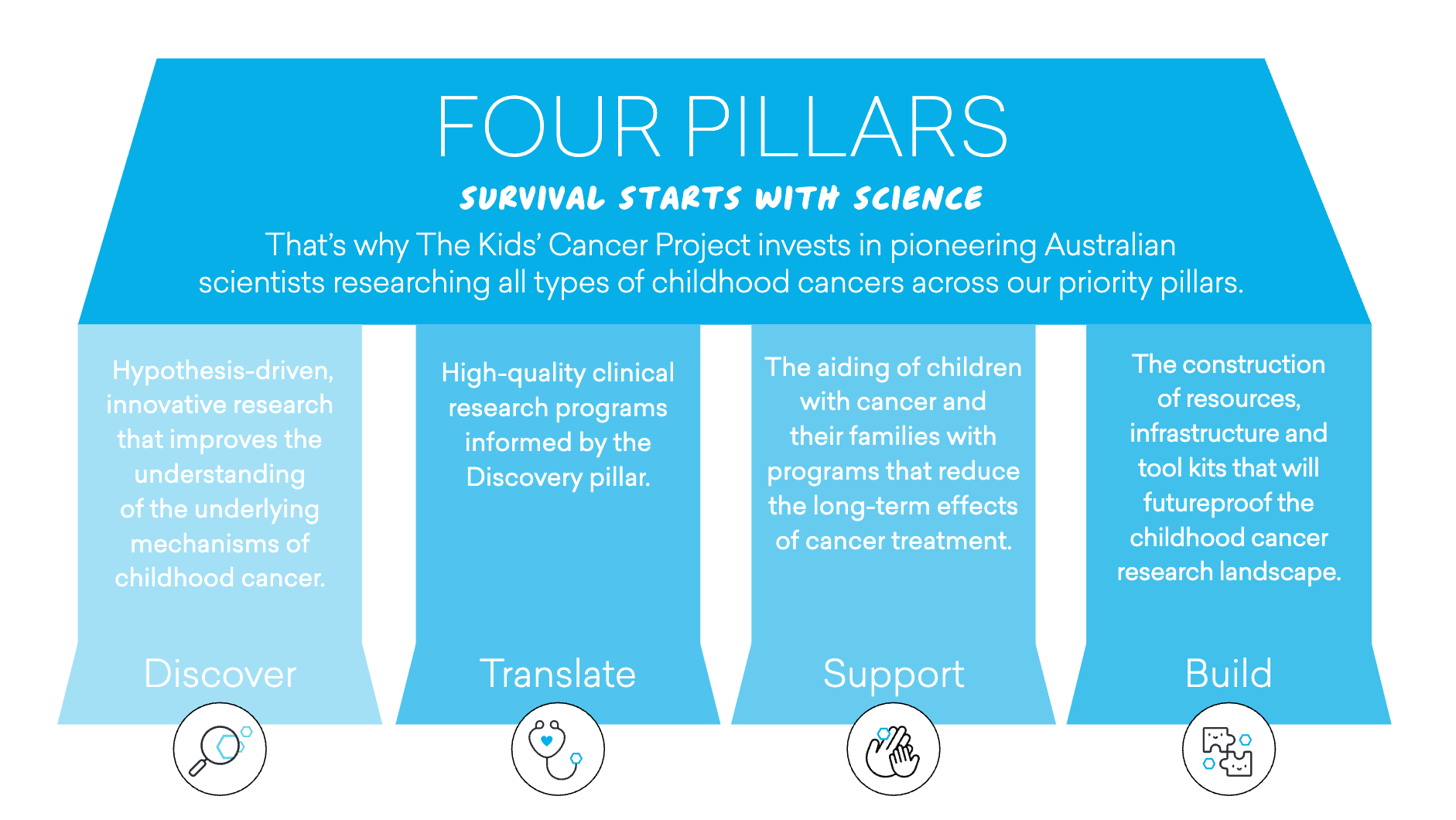
Four strategic research pillars serve as a roadmap for directing funding towards research programs aligned with the strategic priorities and goals.
Discover
Hypothesis-driven, innovative research that improves the understanding of the underlying mechanisms of childhood cancer.
Translate
Taking discoveries and transforming them into high-quality clinical research programs that improve patient outcomes.
Support
Evidence-based research programs that reduce the long-term effects of cancer treatment.
Build
The construction of resources, infrastructure and tool kits that will futureproof the childhood cancer research landscape.
Just like clinical trials, it can take time to make breakthroughs, but even failures are a win. That’s because trial and error is crucial for understanding cancer and treating it correctly. Every misstep is still a success, as it moves the process forward.
The Kids’ Cancer Project believes that the only way no child dies from cancer is through research. A 53 percent improvement in survival rates since our inception is no accident.

